Family Planning
Now, whatever your reason for being interested in family planning, you should select the method that works best for you. Talk with your OB/GYN or Primary Care Provider about your plans for future children, religious or personal beliefs, period symptoms, scheduling concerns (can you remember to take a pill the same time every day?), medical history, and lifestyle choices.
Contraceptive methods are divided up by efficacy. In other words, how well they work at preventing pregnancy. To be clear, no method is 100% perfect. (There are vasectomies that spontaneously reverse. And we’ve all seen the picture of the baby born holding his mother’s IUD.) So you’ll want to look at the advantages and disadvantages of each option and select one that best meets your needs.
Most effective:
The most effective methods remain the “set it and forget it” IUD or implant, as well as permanent solutions like a vasectomy or having your tubes tied (tubal ligation).
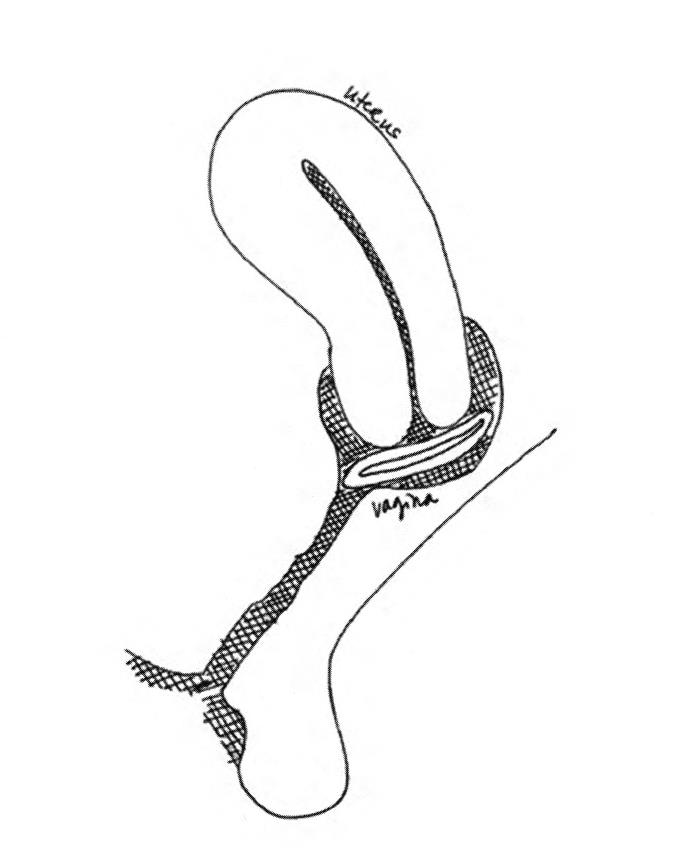
Intrauterine contraception (IUD)
An IUD is a small, flexible, T shaped device. In the United States, we have two options: the copper IUD and an IUD with progestin (Mirena, Liletta, and Skyla).
How does it work?
Once you’ve ovulated and that egg releases into the fallopian tube, pregnancy occurs when the sperm make their way to the egg and fertilize it. The copper IUD releases copper into the uterus. Apparently, copper works as sperm kryptonite. The presence of the copper in the uterus causes an inflammatory response which produces a fluid that is toxic to sperm. Dead sperm = no fertilization = no pregnancy.
Progestin is a synthetic form of progesterone (the hormone builds up and maintains the uterine lining when we are pregnant). Turns out progestin can be very handy at preventing pregnancy as well. Progestin thickens the cervical mucous, making it hard for the sperm to swim through the uterus to that egg. It also thins the uterine lining, making it less hospitable for a fertilized egg. Further, like the copper IUD, this IUD is a foreign body – so there is still that sperm killing inflammatory response.
Interested?
The (non-hormonal) copper IUD can stay in place for 10 years. The most common side effects are bleeding and painful periods.
For progestin IUDs, Mirena can stay in place up to 5 years, Liletta and Skyla can both currently be left in place for up to three years. The most common side effect is irregular bleeding. For many women, their periods become much lighter the longer they keep their IUD inserted — and some women stop having periods completely (which might be welcomed if you are a sufferer of heavy periods.)
Advantages? Very effective, discreet and private, long lasting (3 to 5 to 10 years), lighter periods, and its easily reversed when/if you decide you want to get pregnant. The copper IUD is hormone free.
Disadvantages? The device must be inserted by a healthcare provider, which can be costly, and can be an uncomfortable procedure. There is a small risk of ectopic pregnancy (a pregnancy outside the uterus), and a rare but possible risk for perforating the uterus during insertion.
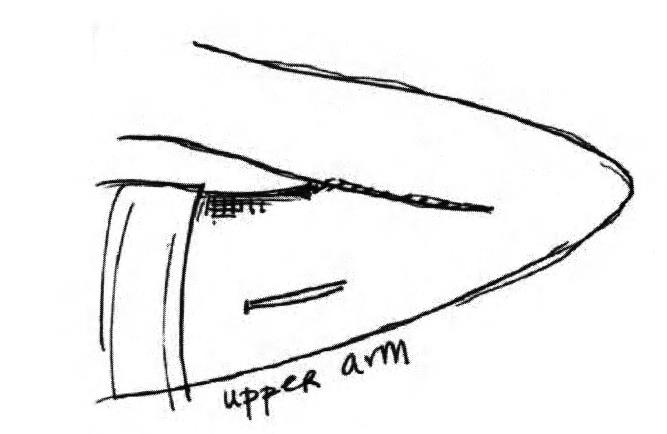
Contraceptive Implant (ie. Implanon, Nexplanon)
An implant is a small rod that is inserted under the skin in your upper arm. It is approximately 4 cm long and 2 mm wide, and is a flexible piece of plastic. Yes, you can see and feel it under your skin, but you probably won’t notice it after placement. But for anyone who has freaked out because they couldn’t feel their IUD strings, feeling the little rod under your skin may be a comfort.
Like the IUD, it is one of the most effective birth control methods, because you don’t have to do anything on a daily or weekly basis. The implant can stay in place for up to 3 years, but if you decide you want to get pregnant sooner, you can have it removed. According to studies, fertility comes back quickly after the implant is removed, and the 1-year pregnancy rates are similar to the rates of women who stopped using condoms or other barrier methods.
Advantages: very effective and lasts up to 3 years.
Disadvantages: it must be inserted by a healthcare provider. Side effects include irregular bleeding and amenorrhea (not having a period), weight gain, and possible bruising and irritation when the rod is inserted. Most women stop using the implant because of the irregular bleeding.
Effective:
Hormone Contraceptives
The most popular forms of birth control are hormone contraceptives (aka, the pill, the patch, and the vaginal ring). These use progestin only (the mini pill or DepoProvera) or a combination of estrogen and progesterone to prevent pregnancy (birth control pills, patch or vaginal ring).
How?
Remember the rise in estrogen back around day 14, which caused a release of LH hormone, and triggered the release of the egg from the follicle? Well, what if your estrogen levels were consistent and you didn’t trigger the release of that egg? No ovulation = no egg available to fertilize = no pregnancy. 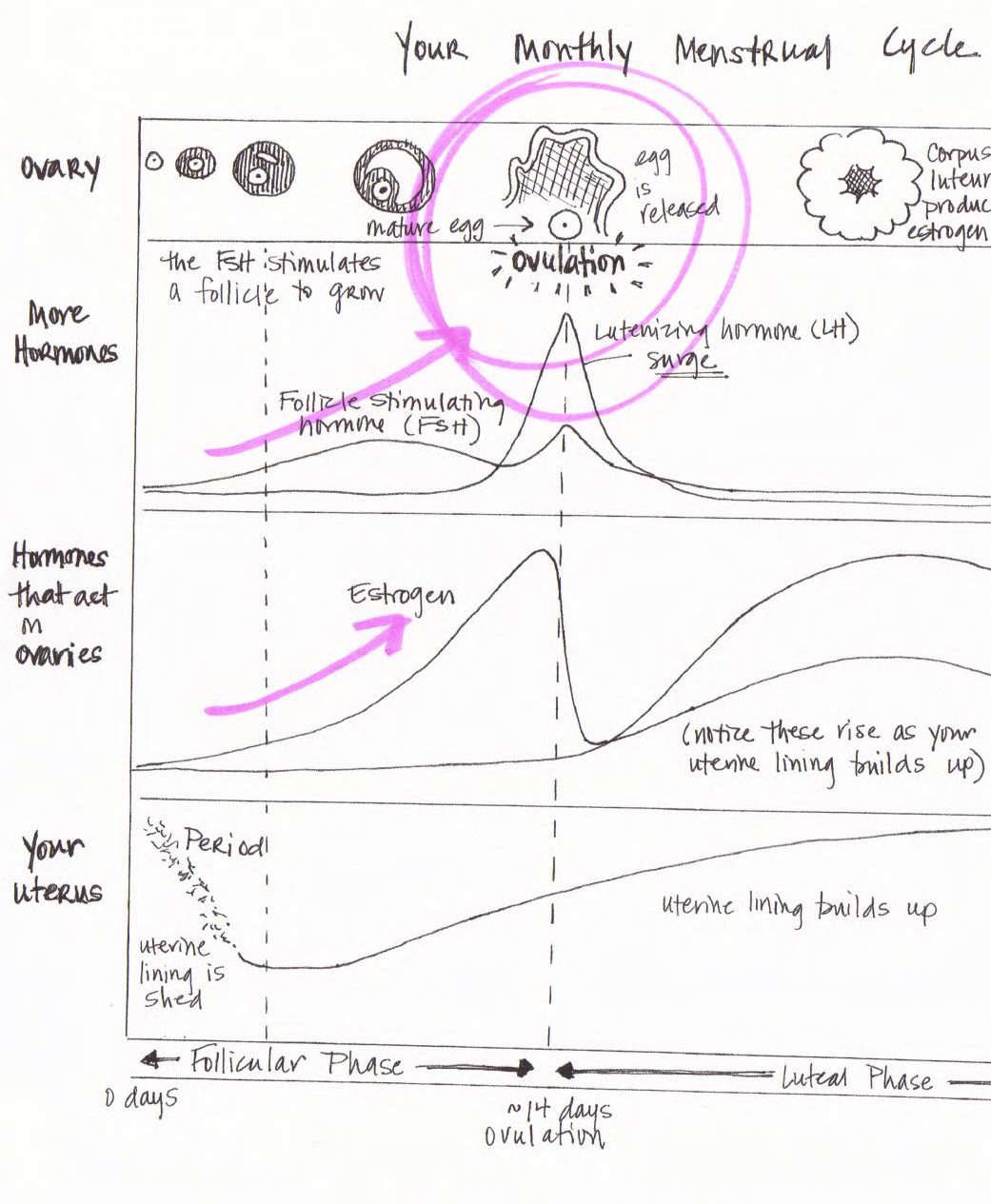 Add the effects of progestin: thickened cervical mucous and thinning of the uterine lining – and you’ve got sperm who are swimming in pudding and no good place to grow an egg in the event that one super-swimmer made it through.
Add the effects of progestin: thickened cervical mucous and thinning of the uterine lining – and you’ve got sperm who are swimming in pudding and no good place to grow an egg in the event that one super-swimmer made it through.
Interested?
The Birth Control Pill (combined hormonal contraceptive)
Probably the most popular, and most well known – the combined hormonal contraceptive “birth control pill” is a pill that you take every day. It is a combination of estrogen and progesterone, and comes in a variety of formulations – some are higher in estrogen, some are lower, some have iron, some have consistent levels of each hormone, and others vary the levels over the course of 21 days. This is where it’s important to speak with your provider about your cycle and symptoms to find the formulation that works best for you.
Most pill packs include 4-7 days of placebo (hormone-free) pills. Your period occurs when you take these pills. Some pills can be taken continuously, so you won’t have a period.
Important Note: since these are synthetic hormones working to suppress ovulation, if you miss two or more consecutive pills, you should use a back up form of birth control.
Advantages? In addition to preventing pregnancy, the pill can help reduce menstrual cramping, acne, and the risk of ovarian and endometrial cancer, as well as iron deficiency anemia.
Disadvantages? Possible side effects include breast tenderness, nausea, bloating, mood changes, breakthrough bleeding or spotting. These typically improve or resolve within two or three months. There is a risk for blood clots or other cardiovascular events, liver or gallbladder disease — so be sure to talk to your healthcare provider immediately if you start having any stomach pain, chest pain, severe headaches, problems with your eyes or severe leg pain and/or swelling in your leg. Some women should not use medications containing estrogen due to increased risk for blood clots or stroke – this includes women over age 35 who smoke cigarettes.
Birth control patch
Similar to the combined estrogen/progesterone pill, the birth control patch works by releasing estrogen and progesterone to suppress ovulation and thicken cervical mucous. But instead of swallowing a pill Every. Single. Day. You apply a patch once a week for three weeks, then leave it off for a week (to have a period).
Important Note: you need to change the site of the patch (buttock, stomach, upper arm, shoulder, back, or hip) each week. No lotions or bandages should be used over the patch.
Advantages: The benefits of the birth control pill, with once a week application.
Disadvantages: It’s visible. It may irritate your skin. It contains estrogen, so if you are breastfeeding, suffer certain types of migraines, or are at risk for blood clots or other cardiac complications, you shouldn’t use this medication. The patch may be slightly less effective in women who are obese.
The Vaginal Ring (Nuvaring)
Like the pill and the patch, the vaginal ring works by releasing estrogen and progesterone to suppress ovulation and thicken cervical mucous. It is highly effective at preventing pregnancy when it is used correctly. The ring is small, flexible, and stays in the vagina for 3 weeks at a time. Your period occurs during week 4 when you remove the ring. The ring can stay in the vagina when you have sex, but you can remove the ring for up to 3 hours if you want.
Important Note: IF the ring is removed for MORE THAN 3 HOURS you should use a backup form of birth control FOR THE NEXT 7 DAYS.
Advantages: Discrete. Stays in place for 3 weeks.
Disadvantages: Side effects are similar to the birth control pill, but some women report vaginal irritation, wetness, and discharge.
Progesterone Only
Injectable contraceptive (DepoProvera)
Depo-Provera is a progestin shot given once every 3 months; it is highly effective at preventing pregnancy. The first dose should be given during the first 7 days of your period, and it immediately works to prevent pregnancy. The most common side effects are irregular bleeding, prolonged bleeding, or spotting. Roughly half of the women stop having periods after 1 year using Depo-Provera.
Advantages? 1 shot every 3 months. Progestin only, so it is safe for women who should not use estrogen.
Disadvantages? It can take about 6 months for your period to come back after you get your last depo injection, which may not be ideal if you’re looking to get pregnant quickly. It may take up to 18 months for fertility to return. Depo has been associated with weight gain. It is also associated with an increased risk for osteoporosis, although this is reversed within 2 years of stopping the injections.
The Progestin Only Mini-Pill
The mini pill does not contain estrogen, making it safe for women who are breast feeding, or who should not take estrogen. When taken AT THE SAME TIME EVERY DAY the progestin only pill is as effective as estrogen/progestin pills, but the failure rate is slightly higher is you are more than 3 hours late when you take it.
How does it work?
The progestin-only pill reduces the amount of cervical mucous and makes it thicker so that sperm can’t swim through it to get to the egg. It is important to note that this change lasts about 20 hours– which is why it is so important to take the pill at the SAME TIME EVERY DAY.
Important Note: If you miss a pill, or are late taking it, you should either abstain from sex for at least two days or use back up birth control (ie. condoms). You can stop using back up after you’ve taken your pill on time for two straight days.
Advantages? The progestin only pill is safe for women who are breastfeeding, or who cannot take estrogen.
Disadvantages? The most common side effects are unscheduled bleeding and changes in your periods. Users have also reported an increase in ovarian cysts as well as acne flares.
Least Effective
The lease effective methods of birth control (resulting in roughly 18 pregnancies per 100 women in 1 year) include barrier methods, spermicides, withdrawal, and the Fertility Awareness Method.
Barrier Methods
Barrier methods (cervical caps, diaphragms, condoms, or sponges) work by blocking sperm from entering the upper reproductive tract, which is where fertilization occurs. Spermicide, which stops the sperm from moving, can also be used to increase efficacy.
Advantages: very safe, reversible, used on-demand (or when you want to have sex), inexpensive, readily available.
Disadvantages: These products need to be inserted/applied before intercourse and may require a certain amount of skill. They do not have the additional benefits of hormonal birth control methods (lighter periods, reduced risk of ovarian and endometrial cancer).
Important Note: diaphragm and cervical cap need to be refitted after pregnancy or delivery.
Fertility Awareness Method:
Fertility Awareness Methods (aka: “natural family planning” or “rhythm method”) use physical signs (temperature, mucous) and/or the calendar to help you determine when you are ovulating. You would then avoid having intercourse or use barrier methods during fertile times. These methods are 77-88% effective at preventing pregnancy, and are most effective when used correctly and when combined with other fertility awareness methods.
How does it work?
Fertility Awareness Methods (FAM) for preventing pregnancy rely on your physiological changes during the menstrual cycle, the periods of fertility and infertility within each cycle, only one ovulation with each menstrual cycle, an egg that can only be fertilized 12-24 hours after it is released from the follicle, and sperm that can live 3-5 days in the cervical mucous and upper genital tract.
Fun Fact: These methods can also be used (in reverse) to improve your chances of conceiving.
The Temperature Method: Your basal body temperature fluctuates throughout your menstrual cycle. It rises about half a degree Fahrenheit when you ovulate and stays elevated for about 10 days. It is important to note that this rise signals the END of the fertile period. To use this method, you need to take your temperature (oral or rectal) FIRST THING IN THE MORNING, EVERY DAY. Keep a log of this temperature on a fertility awareness chart (also available from your doctor or family planning clinic.) Because temperature changes are very small, be sure to get a large scale basal thermometer. You should chart your temperature for about 3 months before using this as a birth control method. For more information visit Fertility United Kingdom.
The Cervical Mucous Method:
Your cervical mucous changes in appearance and consistency throughout the course of your menstrual cycle. In the three to four days immediately before, during and immediately after you ovulate, the mucous is abundant, clear, wet, and stretchy. You would avoid having sex (or use barrier methods) during these fertile days. To use this method, you’ll need to check your cervical mucous every day and chart your findings. You should do this for at least one cycle before using this method as birth control. For more information visit Billings Life or Creighton Model FertilityCare™ System.
The Calendar Method:
Ovulation typically occurs in the 4 days before or after the mid-point of your cycle (ie. day 14 in a 28 day cycle). To use this method, you’ll need to keep a log of when your periods start, for at least 6 cycles. After 6 months of tracking, you evaluate the length of your cycles and use calculations to figure out your “safe (little risk of getting pregnant)” and “unsafe (higher risk of getting pregnant)” days. This method should not be used if your cycles are less than 26 days, have PCOS, are post-partum, breastfeeding (and not getting a period), or transitioning into menopause. For more information visit the Georgetown University Institute for Reproductive Health.
These methods can be hard to learn on your own, so speak with your PCP or family planning counselor if you are considering them as options.